|
Rapists, child molesters and pedophiles served in positions of trust
inside state-licensed addiction treatment centers because, in
California, no criminal background checks were required.
Addiction
counselors preached abstinence to clients even as they racked up fresh
drug and alcohol charges of their own; no system for reporting new
offenses existed.
State
regulators overseeing the rehab industry often failed to catch
life-threatening problems and, when they did, failed to follow up to
ensure that dangerous practices ceased.
These
blistering critiques of California’s weak regulation of addiction
treatment — delivered in a pair of reports from the Senate Office
of Oversight and Outcomes more than four years ago — indicted a system
that far too often produced deadly results for people at perhaps the
most vulnerable point in their lives.
Shortly
after the reports were written, the agency overseeing rehabs ceased to
exist, its responsibilities transferred to a different department. Hopes
ran high that California would modernize its approach to better protect
those who need help. Since then, some has changed for the better —
but much has changed for the worse:
• As
opioid addiction has soared, inexperienced and unscrupulous rehab
operators have rushed in to take advantage of mandatory mental health
treatment coverage required by the Affordable Care Act.
•
California’s notoriously hands-off approach to regulating the industry —
still predominantly non-medical even as other states push hard for a
more medical approach to care — makes it easy for almost anyone
to open a treatment center and bill insurance companies hundreds of
thousands of dollars per client.
•
California’s easy-enroll health insurance marketplace also has helped
cement the state as a go-to destination for addicts seeking to get clean —
or cash in — on what has become known as the Rehab Riviera.
•
Residential treatment facilities bring chaos to neighborhoods and swell
the homeless population with rehab rejects who are kicked to the curb
when their insurance runs dry.
•
Addicts trying to get clean — and their families — often
mistake California’s non-medical rehabs for facilities that provide
medical treatment, thanks in part to slick advertising. In non-medical
facilities, many are dying for want of proper medical care.
Since
the Southern California News Group’s investigation of the Rehab
Riviera began last winter, criminal probes of industry players have been
confirmed by the Federal Bureau of Investigation and several local
district attorneys, including those in Orange and Riverside counties.
The California Department of Insurance is investigating irregularities
as well.
But
proposed laws aimed at closing loopholes in the regulatory system —
such as forbidding patient-brokering, the buying and selling of
well-insured addicts to the centers willing to pay the most for them —
have languished or died in the Legislature.
The
department charged with regulating the industry has advanced no
comprehensive plan to lawmakers to help correct problems that fester in
plain sight.
And as
lawmakers debate where rehab inspectors should be stationed, the
qualifications of drug counselors and how many rehabs should be allowed
per block (many are in ordinary tract houses in residential
neighborhoods) they don’t address the decidedly non-medical nature of
much addiction treatment in California.
“This
is a crisis and it’s growing,” said Mike Pearce, whose daughter,
Shannon, floated in and out of treatment centers until she was killed
Dec. 16 at the Santa Ana apartment she shared with another recovering
addict.
“The
governor should take the direct lead on this…It’s going to take
inspired leadership at the top. And we haven’t had inspired leadership
for a long, long time,” Pearce said.
“It
just galls me that they don’t care.”
Shannon
might still be alive if she had gotten some kind of care from the people
she turned to in faith, Pearce said. She seemed to be making progress
with one counselor, he said, until that counselor relapsed.
“Something
is seriously wrong with how we’re approaching this, and we’re not
confronting it,” said Walter Ling, professor of psychiatry and
founding director of the Integrated Substance Abuse Programs at UCLA.
“There is no leadership. We know it’s not working. We’ve known
that for years.”
Buck stops nowhere
While
governors in other states — Vermont’s Peter Shumlin, Ohio’s
John Kasich, Florida’s Rick Scott — have unveiled aggressive
plans to fight drug addiction and reform the treatment industry, Gov.
Jerry Brown has largely declined to engage.
When
the Southern California News Group summarized its findings for Brown —
including the deaths of at least a dozen people in non-medical detox
facilities, which are not allowed in several other states because of the
extreme health risks posed by withdrawal — the governor’s press
secretary, Ali Bay, said, “I don’t expect our office will have
additional information for you.”
The
department that Brown’s office referred us to for answers, the
Department of Health Care Services’ Substance Use Disorder Compliance
Division, is headed by Marlies Perez.
This
year, Perez’s department is rolling out a system to bring
medication-assisted treatment to California’s hard-hit northern
reaches. It also has hired more inspectors. But addressing the problems
outlined by the Southern California News Group’s probe are not her
department’s purview, she said.
“Our
authority is around the licensing of the facilities. Patient-brokering
is not within our jurisdictional authority. That’s the jurisdiction of
the Department of Insurance. And the state department that oversees
managed health care, that is not with the Department of Health Care,”
she said.
Nor is
it her department’s job, as the state’s regulatory experts, to bring
reform proposals to lawmakers. “We have the opportunity to weigh in on
bills and things brought forward, but the ultimate authority is going to
lie with the Legislature and the governor to make those decisions,”
Perez said.
Over
in the Legislature, several lawmakers are seeking reforms, without much
success.
A bill
that would forbid patient brokering was introduced by Sen. Steven
Bradford, D-Gardena, but stalled in committee over the summer. It has
been amended and awaits a new hearing.
Criminal
background checks are required for acupuncturists, dental hygienists,
optometrists and veterinarians, but substance abuse counselors can work
with vulnerable addicts for five years without officials probing their
background, noted a bill by Assemblyman Reggie Jones-Sawyer, D-Los
Angeles. His bill requiring such screening was overwhelmingly approved
by the Assembly, but stalled in the Senate.
A bill
by Sen. Tony Mendoza, D-Artesia, seeks to address over-concentration of
rehab centers by requiring at least 300 feet between new facilities –
a distance critics say should be at least twice that. A hearing is set
for that in January.
Sen.
Pat Bates, R-Laguna Niguel, sought a study examining whether sober
living group homes should be licensed if they provide counseling, manage
a resident’s schedule or do urine tests to ensure a drug-free
environment. That effort stalled, and her bill has been amended to ask
the Department of Health Care Services to figure out how to evaluate
neighborhood complaints about over-concentration; determine how many
rehab facilities are actually needed in the state; and figure out how to
track their outcomes.
Assemblywoman
Sharon Quirk-Silva’s bill placing a state complaint investigator
directly in Orange County — home to the highest concentration of
licensed rehabs in the state — faced stiff opposition. “The
system right now isn’t broken,” said Sherry Daley of the California
Consortium of Addiction Programs and Professionals at a public hearing.
Quirk-Silva’s bill has been amended, but no hearing has been scheduled
yet.
“You’re
right to feel as if the (issue) isn’t being resolved in a satisfactory
way,” said Quirk-Silva, D-Fullerton. “It’s frustrating.”
Part
of the problem is that too many people are profiting from the current
setup, she added.
“I
think there is some pushback from the addiction centers. They don’t
want to see these programs closed. They’re still making money.”
Treatment
in a non-medical facility can reap $3,410 per day, with monthly bills
topping $100,000 for some clients, according to documents filed in
court.
A
woman from Washington state ran up a $416,050 bill over several months
of treatment with San Clemente-based Sovereign Health.
Some
critics even suggest the basic model of the rehab industry isn’t
focused on wellness.
“There
is no money in sobriety,” said Dave Aronberg, state attorney for Palm
Beach County, Florida. “There is no incentive to recover in this
process. It will cost you your free housing, your free illegal gifts,
your friends. And now you have to move back home to live with Mom and
Dad and find a job.
“But
the insurance benefits will renew, and the cycle will start again if you
just test dirty. Because you can’t be denied coverage for a
pre-existing condition,” Aronberg added.
“Instead
of a recovery model, we have a relapse model.”
Community chaos
Much
addiction treatment in California happens in 6-bed homes in residential
communities.
Neighbors
of such facilities have, for years, complained about the chaos these
homes bring, but those complaints often are dismissed as NIMBY —
“not my backyard syndrome.” And because rehab homes are legally
protected under the Americans With Disabilities Act they don’t need
special permits to operate, leaving neighbors with little recourse.
Records
obtained by the Southern California News Group show that police and
emergency workers in Southern California routinely respond to complaints
connected to state-licensed, neighborhood rehabs. Calls come in for
rape, assault, suicide, attempted suicide, burglary, public
intoxication, child endangerment and indecent exposure, among others.
In
Pasadena, since 2012, police responded to 1,666 calls for service at
just 17 rehab addresses. Those included 91 mental health-related calls,
33 public intoxications, 16 sex offender registrations, 16 burglaries, a
dozen vehicle thefts, 11 batteries, four overdoses, two indecent
exposures, and one each of assault with a deadly weapon, lewd conduct,
prostitution, and child endangerment, according to call logs.
In the
eight south Orange County cities patrolled by the Orange County
Sheriff’s Department, there were 2,500 calls for service during that
same period. The heaviest-hit were San Clemente, where there were 926
calls, the majority to just six addresses; and San Juan Capistrano,
where there were 667 calls, the majority to just 10 addresses.
In the
city of Riverside, there were 1,052 calls for service at 26 licensed
rehab centers, including 186 mental health-related calls, 18 overdoses,
five sexual assaults, three rapes, one alleged child molestation and one
felon with tear gas. A single center on Brockton Avenue generated 285
calls for service.
“The
addicts in these facilities are not getting helped, they’re getting
hurt,” said Warren Hanselman of Advocates for Responsible Treatment, a
group pushing for better regulation in San Juan Capistrano.
Political will
Richard
Rawson spent years advising California on how to best regulate addiction
treatment as co-director of UCLA’s Integrated Substance Abuse
Programs.
“The
state drug and alcohol office never has been a particularly powerful
entity,” said Rawson, now retired. “I suspect that’s because
there’s not a lot of political support for getting out and cleaning up
this industry.”
It is
different in Rawson’s home state of Vermont. “Here you had Gov.
(Peter) Shumlin in 2014 doing his entire State of the State speech on
opioid addiction. It became the top priority in the state government.
That has never happened in California – there’s too much other stuff
going on.”
Perez,
head of the Substance Use Disorder Compliance Division, deserves credit
for channeling California’s entire $90 million federal grant toward
expanding medication-assisted treatment in hard-hit corners of the
state, Rawson said. But without leadership from the top, he added,
it’s hard to get more done.
“The
mess in the rehab industry is a problem that politicians seem to want to
avoid.”
Huntington
Beach filmmaker Greg Horvath produced a documentary, “The Bu$iness of
Recovery,” to expose what he calls the “gross deficiencies”
addiction treatment.
“The
industry must change,” said Horvath. “There must be oversight and
regulations in place that protect the public and the families who are
entrusting these centers with their loved ones. Treatment needs to be
more scientific and empirically validated. The educational requirements
for people treating addiction must be higher.”
UCLA
psychiatrist Ling agrees, suggesting much of the industry is built on
false claims: “This is a very critical point: There is a
misrepresentation of what they do because they make people believe they
are rendering medical services.”
Florida,
hard-hit by pill mills and deadly fraud in the treatment industry,
responded to this disconnect with new laws criminalizing dishonest
marketing, kickbacks and patient-brokering.
“We
shut these places down because the government had the courage to do
so,” said Aronberg, state attorney for Palm Beach County.
On
Wednesday, the state of New York launched a new ad campaign to alert
those seeking help about bogus rehab referral services. “Vulnerable
New Yorkers struggling with addiction are being targeted and falsely
promised life-saving treatment services and then are given inadequate
and ineffective treatment at outrageous costs,” Gov. Andrew Cuomo
said.
Fixing
California’s regulatory ills would require a significant overhaul of
the system, said Harry Nelson, founding partner of Nelson Hardiman, a
firm specializing in health care law. He’s not sure there’s an
appetite for it.
“The
problem is, drug rehab is complicated, so it doesn’t fit neatly into
the healthcare category or the community care framework,” Nelson said.
“It has been cut off from the rest of the health care system for so
long it has had a silo effect.”
Undoing
that isolation — by integrating addiction treatment into the
mainstream health care system — will ultimately address
irregularities, said Martin Y. Iguchi, a senior behavioral scientist at
the RAND Corporation and professor in the departments of Psychology and
International Health at Georgetown University.
“When
you have fraud like that, that’s because of the Wild West nature of
the programs that have popped up,” he said. “There hasn’t been a
lot of attention paid because, without funding flowing, nobody seemed to
really care. The more these programs are part of the traditional
(health) care system, the better off everyone will be.”
Said
Keith Humphreys, director for mental health policy at Stanford
University’s Department of Psychiatry and Behavioral Sciences:
“These problems are not common in oncology.”
Solutions
The
Southern California News Group has talked to hundreds of people about
how to address problems in rehab industry, and reviewed thousands of
pages of regulatory documents and academic studies. Some recommendations
from experts include:
•
Establish national accreditation standards for all addiction treatment
facilities and programs that reflect evidence-based care.
•
License addiction treatment facilities as health care providers.
•
Collect patient outcome data and make it available to the public.
•
Mount a national health campaign educating people about medical
responses to addiction and improve addiction treatment training in
medical schools.
•
Tighten up truth-in-advertising laws to rein in call centers that
intercept and broker patients to facilities that pay them.
•
Require more formal education, criminal background checks and state
licensing for addiction counselors and those who work in treatment
centers.
•
Expand the state’s power to license, regulate and shut down
facilities.
•
Tighten the special enrollment period for buying health insurance,
making it harder to do mid-year enrollments.
•
Forbid financially interested third-parties from paying health insurance
premiums, except for parents.
•
Just as Medicare rewards good hospitals for not having readmissions,
insurers can do same for addiction treatment providers. “Pay the good
ones more and the bad ones less,” said Florida state attorney Aronberg.
“It
is long past time for (the rehab industry) to catch up with the science.
Failure to do so is a violation of medical ethics, a cause of untold
human suffering and a profligate misuse of taxpayer dollars,”
concluded the National Center on Addiction and Substance Abuse at
Columbia University.
Ling,
of UCLA, believes California can start small — by appointing a
commission to review how things are done, and how they might be done.
By Teri Sforza
| tsforza@scng.com, Tony Saavedra
| tsaavedra@scng.com and Scott Schwebke
| sschwebke@scng.com | Orange County Register
https://www.ocregister.com/2017/12/29/rehab-riviera-industry-struggling-to-get-clean/
|
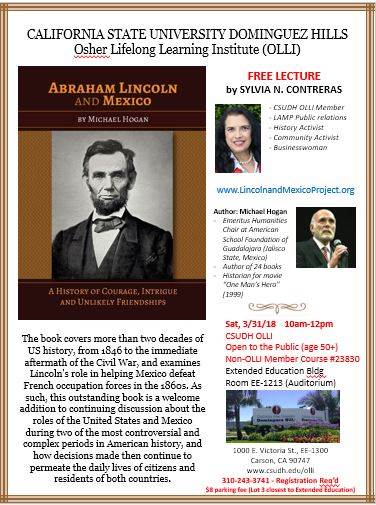
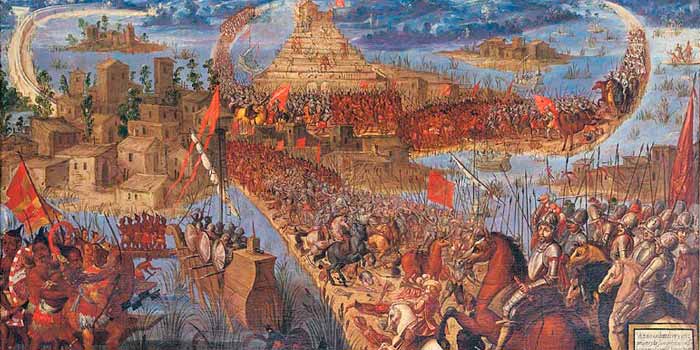
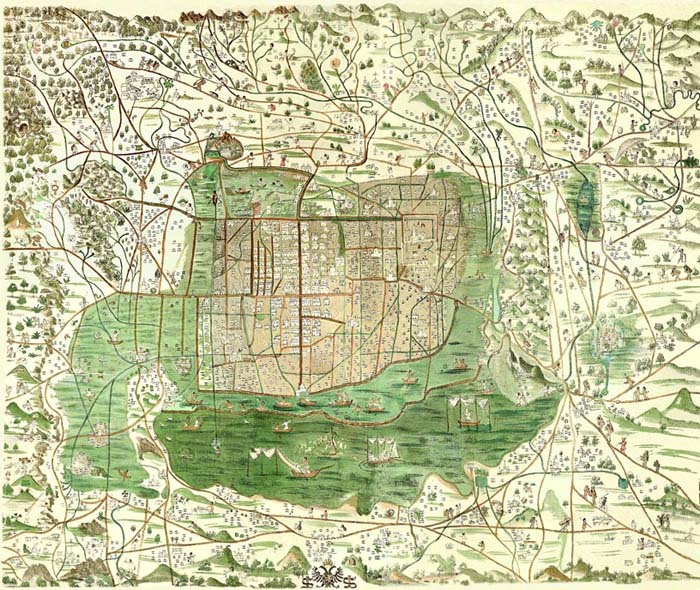
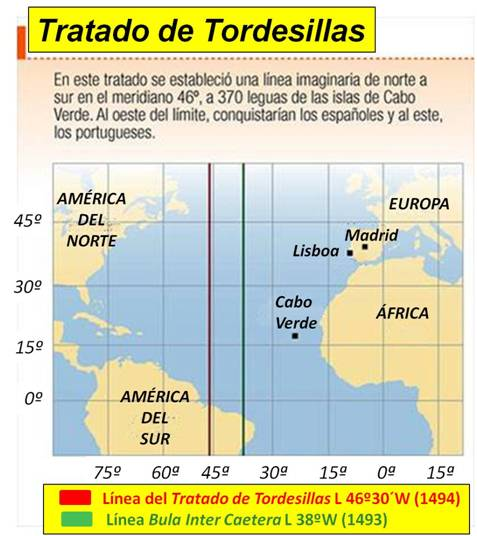
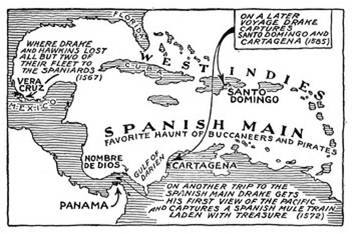
 The
book inspired launching “Lincoln and Mexico Project” (LAMP) in
2016-17 reaching across the U.S.A. with representatives in
Guadalajara, Mexico; Los Angeles, CA; San Diego, CA; New York, New
York; Austin, Tx; and Chicago, IL. A few of LAMP’s goals are:
1) promote better relations between the U.S.A. and Mexico, 2)
integrate the book’s education into high schools and university
curricula, 3) bring the history “Abraham Lincoln and Mexico” to
the general audience. It seemed such an important movement, I
began volunteer efforts in Spring 2017. For additional
information, please visit: https://lincolnandmexicoproject.wordpress.com/about/
The
book inspired launching “Lincoln and Mexico Project” (LAMP) in
2016-17 reaching across the U.S.A. with representatives in
Guadalajara, Mexico; Los Angeles, CA; San Diego, CA; New York, New
York; Austin, Tx; and Chicago, IL. A few of LAMP’s goals are:
1) promote better relations between the U.S.A. and Mexico, 2)
integrate the book’s education into high schools and university
curricula, 3) bring the history “Abraham Lincoln and Mexico” to
the general audience. It seemed such an important movement, I
began volunteer efforts in Spring 2017. For additional
information, please visit: https://lincolnandmexicoproject.wordpress.com/about/










 Now that you’re on our website, you have already
taken a step in the right direction. There are many things from
here that you can do. You can start by becoming a member. There
are two different types of membership, donor and sponsor. As a
donor member you will be supporting the development of the HDC,
‘Living History Museum’ Projects and of course, our horses.
Upon donation to any of these categories you will receive a letter
with explanations of what your donation has done for the
Now that you’re on our website, you have already
taken a step in the right direction. There are many things from
here that you can do. You can start by becoming a member. There
are two different types of membership, donor and sponsor. As a
donor member you will be supporting the development of the HDC,
‘Living History Museum’ Projects and of course, our horses.
Upon donation to any of these categories you will receive a letter
with explanations of what your donation has done for the























 Dorothy
Lamour was one of the top movie
stars. Her genre was South
Pacific themes. Lamour
wore sarongs in 14 films.
Perfect timing. Dad always
resourceful was able to get some
walk on jobs as an extra for
mom.
Dorothy
Lamour was one of the top movie
stars. Her genre was South
Pacific themes. Lamour
wore sarongs in 14 films.
Perfect timing. Dad always
resourceful was able to get some
walk on jobs as an extra for
mom.  With
my sister in school, Dad brought
home a big rabbit, I think as
company for me. Scottie
enjoyed the new attraction
in the neighborhood.
Scottie would clear the low
fence easily and chase the bunny
all around the yard. They
would take a rest, nestled next
to each other, and then
start the race all over again.
They became good friends.
This is what I remember Bunny
looked like.
With
my sister in school, Dad brought
home a big rabbit, I think as
company for me. Scottie
enjoyed the new attraction
in the neighborhood.
Scottie would clear the low
fence easily and chase the bunny
all around the yard. They
would take a rest, nestled next
to each other, and then
start the race all over again.
They became good friends.
This is what I remember Bunny
looked like.


































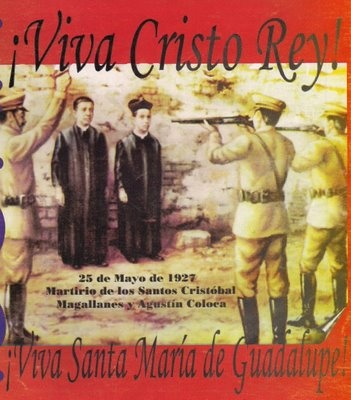

 And,
every time Papá and I
went walking across the
river to Nuevo Laredo to
buy groceries or to get
a hair cut, he would
stop by the church to
say hello to Father
Lozano. The church
was just one block away
from the International
bridge. Father
Enrique Tomás Lozano
became well known in
Nuevo Laredo and Laredo
because he converted an
old building next to his
residence and made it
into a safe haven for
orphaned boys that he
called his beloved
"pelones."
He shaved their hair for
hygienic reasons.
He was very proud of
them. And, most
importantly, he sent
many of them to
Monterrey, Mexico, to
continue their
education, and some
became doctors,
engineers,
lawyers, and teachers.
And,
every time Papá and I
went walking across the
river to Nuevo Laredo to
buy groceries or to get
a hair cut, he would
stop by the church to
say hello to Father
Lozano. The church
was just one block away
from the International
bridge. Father
Enrique Tomás Lozano
became well known in
Nuevo Laredo and Laredo
because he converted an
old building next to his
residence and made it
into a safe haven for
orphaned boys that he
called his beloved
"pelones."
He shaved their hair for
hygienic reasons.
He was very proud of
them. And, most
importantly, he sent
many of them to
Monterrey, Mexico, to
continue their
education, and some
became doctors,
engineers,
lawyers, and teachers.